Treating Pandemic Stress and Pain with Acupuncture
Imagine if you will, a smoke alarm that won’t stop going off. One of two things might happen. You’d either eventually attenuate to it and not notice any alarms or you’d become hypersensitive and completely on edge— jumping at every little sound. We don’t want to live in a world where alarm bells are constantly ringing but we also don’t want to rip the smoke alarm out of the wall either. Now imagine that a ball or a bird is flying towards your head—You tense in anticipation. Then, the object either hits or misses you, at which point you’d physically relax as the threat has passed. But what can you do if the threat isn’t physical? In this case, the body doesn’t always receive the signal that the threat has passed and therefore doesn’t know to relax. What then? That’s where acupuncture comes into play.
How does stress affect the body?
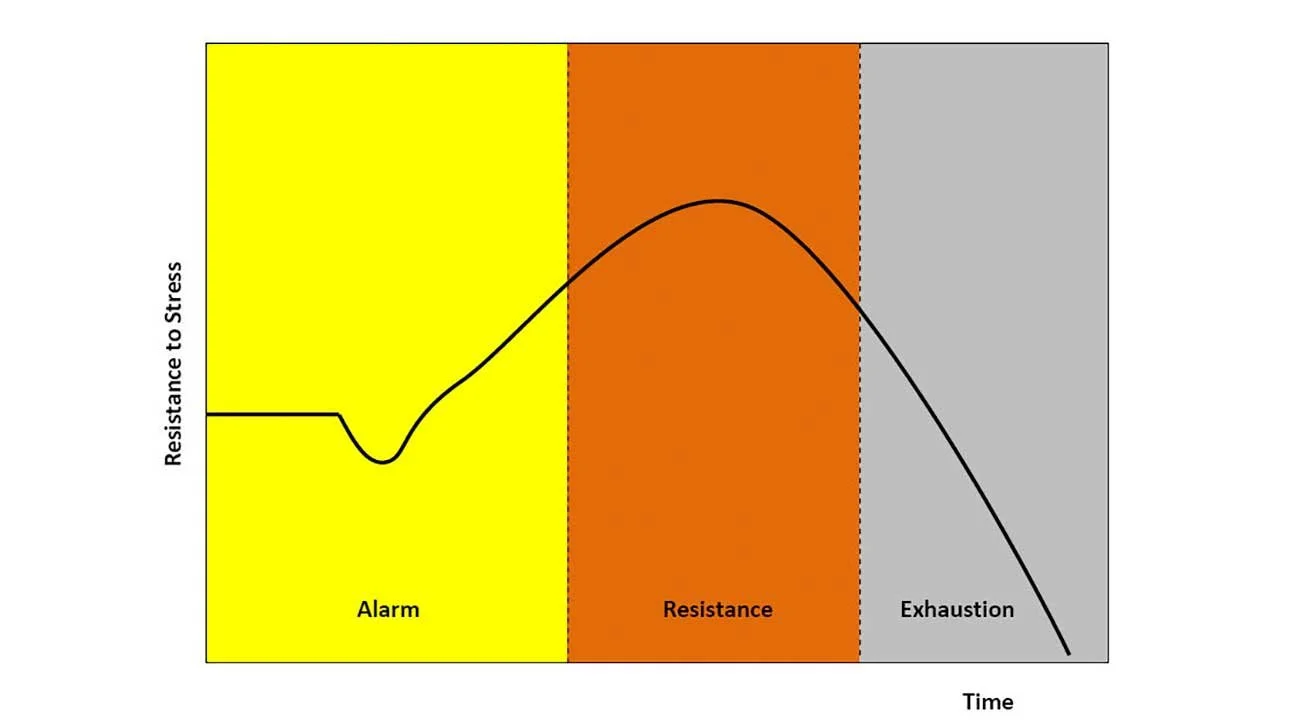
Stress and stressors on the body are helpful in the short term. The alarm clock, the morning sun, will increase cortisol and get us out of bed and ready to start the day. An unexpected car horn may give us enough adrenaline to cross the street quickly, increasing blood flow to muscles and the heart’s ability to get oxygen to those muscles. Strength training and exercise are other good and necessary stresses on the body that build up our resistance over time. The body’s short-term response to stress, pain, and yes even the idea of a painful or stressful situation is one that in a perfect world returns to a state of homeostasis after the threat has passed. The body's flight, fight, or fawn cycle should be complete and return to neutral (Duncan, 2019). But what happens when the danger doesn’t pass, what happens almost 2.5 years into the COVID-19 pandemic? What happens when we push beyond our zones of resiliency. We know that chronic stress will result in very real biological responses that can alter our ability to bounce back over time. “Recent studies have revealed heightened levels of anxiety and depression during the ongoing pandemic, with specific factors such as social or lower economic resources influencing stress perception (Pfeifer et al., 2021).”
So what can happen with prolonged chronic stress?
“Prolonged or exaggerated response to pain or non–pain-related stressors may intensify sympathetic and neuroendocrine activity, exhaust cortisol, and perpetuate widespread pain and inflammation. Elevated cortisol levels following acute stress may facilitate the consolidation of fear-based emotional memories and condition a sensitized physiologic stress response.”
In other words, chronic stress can lead to chronic pain and get stuck in a cycle. This in turn leads to widespread inflammation, depletion of serotonin, or increased autoimmune hypersensitivities (Hannibal & Bishop, 2014). Clinically, in addition to chronic pain, I’ve seen an uptick in menstrual irregularities, insomnia, digestive issues, migraines, and headaches, usually with accompanying neck or low back pain.
How can we relate this to acupuncture?
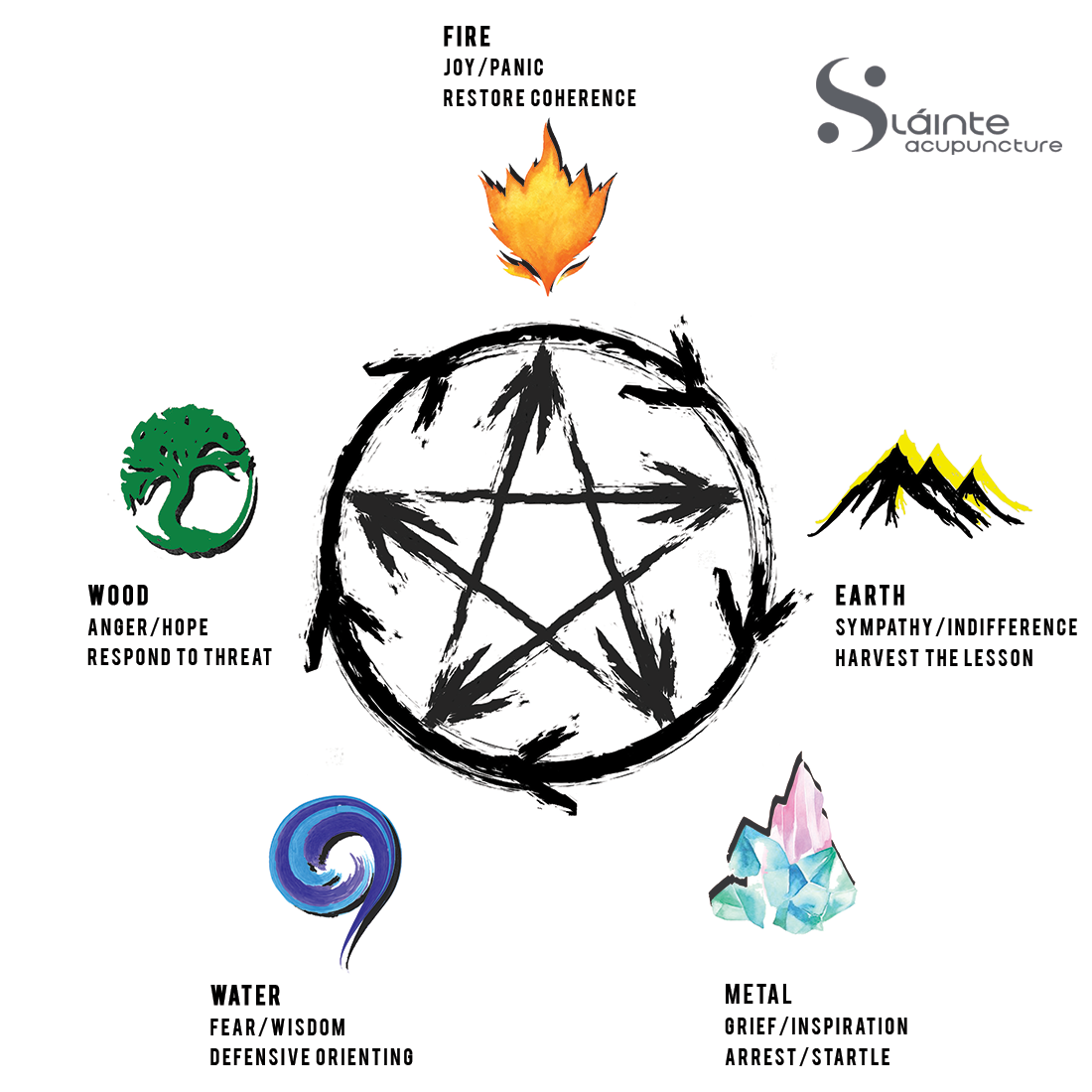
Acupuncture has the unique ability to help the body complete the stress cycle. This allows for a break in the pain cycle and a return to a state of self-regulation by concurrently addressing the physical and emotional body. Alaine Duncan’s work, The Tao of Trauma relates the body's Self Protective Response to the Taoist Five Elements. One example of this is the association of fear with the water element and in turn the kidneys. If we relate this to the body’s adrenal response and the HPA-Axis, there is a perfect correlation and marriage of eastern and western perspectives. As discussed above we can deplete and exhaust cortisol in the body, just as we can over boil a pot of water and start to burn the pot itself. This can be applied to the kidneys' effect on the heart and the heart's effect on the kidney, in other words, the relationship between fire and water or joy and fear.
Image: 5 Element Generating and Control Cycle
Image: Sláinte Acupuncture 2022
“East Asian Medicine incorporates the external environment and emotional landscape into its orthopedic assessments.”
Our bodies are hardwired for survival. Over time, our brains have evolved methods of interpreting, cataloging, and maintaining information to keep us alive. This survival-based hardware is intriguing and very necessary. All of these unconscious biological processes are very much tied into how much we perceive our environment to be safe. The last few years have taken a toll on our emotional and physical well-being. An important point to remember is that these stressors, threats, or perceptions of danger, whether real or imagined, have a very real physiological response. It’s why watching scary movies can be fun, but also cause very real muscle contractions when the jump scare occurs (Tremblay, 2019). It is also why East Asian Medicine incorporates the external environment and emotional landscape into its orthopedic assessments.
It’s why I refer to my practice at Sláinte Acupuncture as integrative. There does not have to be a hard divide between western science and eastern medicine. Acupuncture is a powerful modality that can help regulate the physiological and in turn the emotional body by helping to regulate the nervous system back to a place of healthy regulation.
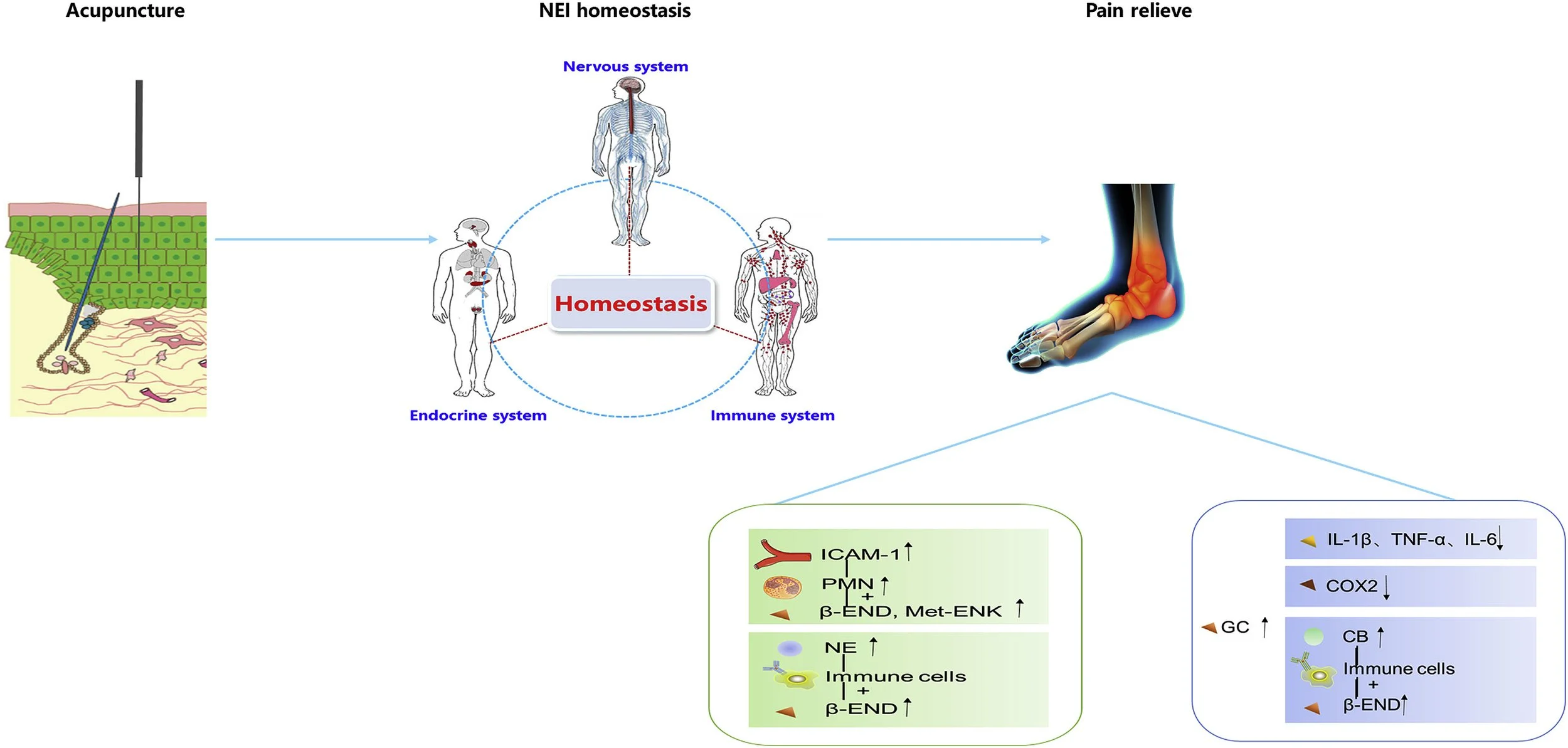
How can acupuncture help to regulate the sympathetic nervous system?
I do this in a few ways. The first is through asking. I do a thorough intake of medical history. I specialize in orthopedics but want to know about the internal environment and how the whole system functions. Because the ultimate goal is one of homeostasis and resiliency (Xu et al., 2018). Patients often think they have to separate orthopedic concerns from internal issues regarding sleep, digestion, elimination, and menstruation. Somatovisceral and visceral-somatic pathways or the way the body affects the organs and the way the organs affect the body are a topic for another essay but know that an informed practitioner is treating the whole person and not just one symptom.
Anxiety does not cause stomach aches; rather, feelings of anxiety and stomach aches are both
ways that human brains make sense of physical discomfort. There is no such thing as a purely
mental cause, because every mental experience has roots in the physical budgeting of your
body. This is one reason physical actions … can be surprisingly helpful in addressing problems
we traditionally view as psychological. (Barrett, 2020)
The next way is through palpation or touch. By palpating the channels and cross fiber palpating muscles, I can find areas of excess or deficiency or hyper or hypotonicity in the muscles. One way that stimulating acupuncture points, on a micro level can help to act on a macro level, is by acting as the stimulus in which our body gets stuck anticipating. It can also stimulate a motor point or trigger points, elicit neuromuscular fasciculations, and reset a muscle to its appropriate length. Especially if the muscle is stuck short or long often bracing or in anticipation or inhibited in firing due to pain avoidance (Ellingsen et al., 2018).
“A variety of pathways play a role when acupuncture is used to treat patients with persistent pain:
The sympathetic nerve pathway
The endocrine and immunity pathway
Image: Promoting the robustness function of acupuncture in treating diseases. (Xu et al., 2018)
#MoreThanJustNeedles
At Sláinte we use needles, yes, but every treatment is custom-tailored in real-time to the patient and how they are responding to treatment. I’m trained in multiple styles of acupuncture and various non-needle techniques so I feel confident that each patient can receive the best treatment for them. This can be through, e-stim or electro-acupuncture, acupressure, somatics, amma massage, tui na, gua sha (or scraping), moxibustion, infrared heat therapy, or cupping. Everybody is different. Every body is different. It’s my job to meet my patients where they are at but to never discount the environment in which they find themselves.
We know touch can be very therapeutic. On the other hand, one common complaint I hear from patients is neck and trap tension that doesn’t resolve with massage therapy, chiropractic, or other manual therapies. This is because without addressing the underlying nervous system, without considering the person in their environment, our bodies will continue to brace and protect our vital organs and vessels. Acupuncture has the unique ability to ground a patient and disengage this process of bracing/anticipation. We bring about parasympathetic regulation through controlled and conscious touch and intervention. By using palpation we can use the body’s real-time feedback to elicit changes in muscle tone and lessen pain at the site of chief complaint with the use of distal acupuncture points before engaging in local intervention. There’s no need to meet trauma with more trauma. The body is sending us these signals for a reason and it is our job to interpret why and gently lead the body back to a place of balance and safety. Think back to the bird flying at your head. Step one is always to get the body to feel safe and relaxed, then the door is open for local intervention with a greater chance for the benefits of the treatment to last.
As pack animals, we regulate and attune our nervous systems with those around us. So resonating with whatever practitioner you choose to work with is just as important as the treatment performed. If you have any questions regarding how acupuncture or any of the above-mentioned modalities might aid you in regulating your nervous system, don’t hesitate to reach out. I can be reached at www.SlainteAcupuncture.com or info@Slainteacupuncture.com
Sláinte: pronounced SLAHN-chə is Gaelic for health. Derived from the old Irish noun slan which means safe, whole, or health, today it is used as a greeting or a toast.
References and Works Cited
Barrett, L. F. (2020, November 23). Your Brain is Not For Thinking. The New York Times. Retrieved July 17, 2022, from https://www.nytimes.com/2020/11/23/opinion/brain-neuroscience-stress.html
Ellingsen, D.-M., Napadow, V., Protsenko, E., Mawla, I., Kowalski, M. H., Swensen, D., O'Dwyer-Swensen, D., Edwards, R. R., Kettner, N., & Loggia, M. L. (2018, November). Brain mechanisms of anticipated painful movements and their modulation by manual therapy in chronic low back pain. The journal of pain. Retrieved July 17, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6220681/
Hampton, T. (2022, February 23). Pandemic Stress and the Brain. Pandemic Stress and the Brain. Retrieved July 17, 2022, from https://hms.harvard.edu/news/pandemic-stress-brain
Hannibal, K. E., & Bishop, M. D. (2014, December 9). Chronic stress, cortisol dysfunction, and pain: A psychoneuroendocrine rationale for stress management in pain rehabilitation. Physical therapy. Retrieved July 17, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4263906/
Pfeifer, L. S., Heyers, K., Ocklenburg, S., & Wolf, O. T. (2021, September 29). Stress research during the COVID-19 pandemic and beyond. Neuroscience & Biobehavioral Reviews. Retrieved July 17, 2022, from https://www.sciencedirect.com/science/article/pii/S0149763421004267
Tremblay, S. (2019, March 2). Your Body on A Horror movie. Sciencing. Retrieved July 17, 2022, from https://sciencing.com/your-body-on-a-horror-movie-13714006.html
Xu, Y., Guo, Y., Song, Y., Zhang, K., Zhang, Y., Li, Q., Hong, S., Liu, Y., & Guo, Y. (2018, February 1). A new theory for acupuncture: Promoting robust regulation. Journal of Acupuncture and Meridian Studies. Retrieved July 17, 2022, from https://www.sciencedirect.com/science/article/pii/S2005290117301401
Zhang, R., Lao, L., Ren, K., & Berman, B. M. (2014, February 1). Mechanisms of acupuncture–electroacupuncture on persistent pain. American Society of Anesthesiologists. Retrieved July 17, 2022, from https://pubs.asahq.org/anesthesiology/article/120/2/482/11811/Mechanisms-of-Acupuncture-Electroacupuncture-on